Dieting is distinguished from diet by an emphasis on a temporary change in eating patterns to achieve short-term goals. If good health is the most important goal, dieting is likely to be counterproductive. This monograph is concerned with the long-term health benefits of fat loss rather than losing weight temporarily to look good for a special occasion. Loss of weight due to a loss of water or lean tissue rather than fat can be harmful to health. Tobacco smoking as a means of curbing appetite is detrimental to health.
The most effective dieting change is one that permanently reduces the rate of calorie consumption. But even people who will exert a great deal of effort to exercise for weight-loss often refuse to apply effort to reduce eating — or to eat less tasty foods that are low in calories, but high in fiber. Instead, most diet & dieting strategies emphasize shifts in relative consumption of the macronutrients: fat, carbohydrate and protein. But for every one of these macronutrients it is a mistake not to pay attention to subcategories. It makes a great deal of difference what type of fat, carbohydrate or protein is being increased or decreased in the diet. Another important distinction is the health objective of the diet: to lose fat, to reduce cardiovascular disease, to prevent diabetes, etc. These objectives are very related, but still distinct.
Dietary fat is very readily absorbed and is readily converted to body fat. It is easy to eat large amounts of fat calories before satiation occurs. The impetus behind low fat diets received a boost in 1961 when the Framingham Heart Study reported correlation between blood cholesterol and heart disease. Saturated fat increases blood LDL cholesterol without affecting HDL cholesterol. Butter (high in saturated fat) consumption declined while margarine (high in trans fat as well as omega−6 polyunsaturated fat) consumption increased. Trans fats lower beneficial HDL cholesterol and increase the LDL/HDL ratio approximately twice as much as saturated fat [NEW ENGLAND JOURNAL OF MEDICINE; Ascherio,A; 340(25):1994-1998 (1999)]. Both trans fats and saturated fats raise plasma insulin and triglyceride levels, suggesting that both types of fats promote insulin resistance [METABOLISM; Ibrahim,A; 54(2):240-246 (2005)].
A low fat diet may be low in the essential omega−3 fatty acids which are part of cell membranes and are highly protective against cardiovascular disease. The omega−3 fatty acid DHA may protect against insulin resistance. While omega−6 polyunsaturated fats can reduce the vulnerability of hearts to fibrillation, they can also promote inflammation, contributing to atherosclerosis.(See Fats you Need and DHA for Hearts and Minds.) "Low fat" foods are frequently high in sugar content, which can elevate blood triglycerides and promote insulin resistance (see below).
An analysis of several studies showed that although low fat diets do not result in less weight loss than low carbohydrate diets after six months, there is no difference after one year. But total blood cholesterol and LDL cholesterol is reduced by a low fat diet [ARCHIVES OF INTERNAL MEDICINE; 166(3):285-293 (2006)]. (Dropout rates from these studies were very high — one-third to one-half.) A study comparing a high-fat diet to a high-carbohydrate diet showed a greater gain in body fat from a high-fat diet over a four year period [THE AMERICAN JOURNAL OF CLINICAL NUTRITION; Eckel,RH; 69(3):440-447 (1999)]. A high-fat meal elevates A HREF="../lifeext/aging.html#inflame" TARGET="_blank">plasma inflammatory cytokines more than a high carbohydrate meal [JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY; Nappo,F; 39(7):1145-1150 (2002)].
Avoiding fat in the diet will not, in general, prevent body fat. Body fat is positively associated with a high variety of dietary sweets, snacks, condiments, entrees and carbohydrates, and is negatively associated with a high variety of vegetables (excluding potatoes) consumed [THE AMERICAN JOURNAL OF CLINICAL NUTRITION; McCrory,M; 83(4):803-808 (2006)].
High blood glucose associated with high carbohydrate consumption can damage the insulin-producing beta cells in the islets of the pancreas — an effect which amplifies the lipotoxicity of high levels of blood lipids [DIABETES; Robertson,RP; 53(Suppl 1):S119-S124 (2004)]. Foods that significantly elevate blood glucose are said to have a high glycemic index. But dietary fructose, which has a low glycemic index, is now being held to be most highly associated with the growth of obesity and type 2 diabetes in recent decades.
Type 2 diabetes (also called "non-insulin-dependent diabetes") was formerly known as "adult onset diabetes". But adolescents have increasingly been developing the disease. A Cincinnati study showed a ten-fold increase in adolescent type 2 diabetes in the period between 1982 and 1994 [THE JOURNAL OF PEDIATRICS; Pinhas-Hamiel,O; 128(5 Pt 1):608-615 (1996)]. There was not a ten-fold change in genetic make-up of adolescents in that period, but there was a great increase in adolescent obesity. A study of nearly 85,000 nurses concluded that obesity is the single most important factor leading to type 2 diabetes in women [NEW ENGLAND JOURNAL OF MEDICINE; Hu,FB; 345(11):790-797 (2001)] — which undoubtedly applies to men also.
When fructose is ingested in large quantities it stimulates the liver to produce triglycerides, it promotes glycation of proteins and it can induce insulin resistance [DIABETES; Faeh,D; 54(7):1907-1913 (2005)]. By failing to elevate insulin and leptin (both of which suppress appetite) fructose can contribute to increased calorie consumption. In recent decades there has been a great increase in the use of High Fructose Corn Syrup (HFCS) in processed foods. From 1970 to 1997 per capita consumption of HFCS increased from 0.5 pounds to 62.4 pounds in the United States [THE AMERICAN JOURNAL OF CLINICAL NUTRITION; Elliott,SS; 76(5):911-922 (2002)]. The increased consumption of HFCS, glucose syrup and sucrose has been blamed for the rapid increase in obesity and type 2 diabetes. HFCS is not only common in ice cream, breakfast cereals and sweet baked goods, but has become the predominant sweetener in soft drinks ("soda pop"). A study of over 50,000 nurses over an eight-year period found that the consumption of one or more soft drinks per day was associated with greater weight gain and nearly double the risk of type 2 diabetes [THE JOURNAL OF THE AMERICAN MEDICAL ASSOCIATION; Schulze,MB; 292(8):927-934 (2004)].
The greatest impetus for low carbohydrate diets (the "low-carb craze") has come from Dr. Robert Atkins and his Atkins Diet. According to Dr. Atkins, a high carbohydrate diet leads to excessive fluctuations in blood sugar and blood insulin leading to over-eating, insulin resistance, obesity and type 2 diabetes. He claimed that diet high in fat and protein would reduce appetite, increase insulin sensitivity, increase HDL cholesterol and reduce triglycerides [ANNALS OF INTERNAL MEDICINE; Boden,G; 142(6):403-411 (2005)]. In the absence of dietary blood sugars from carbohydrates the body is forced to burn fat.
The "low carb diet" does not adequately distinguish between types of fats or types of carbohydrates. Saturated fat can increase insulin resistance [THE AMERICAN JOURNAL OF CLINICAL NUTRITION; Parker,DR; 58(2):129-136 (1993)]. Even a high ratio of omega−6 to omega−3 polyunsaturated fats may promote insulin resistance [LIPIDS; Storlien,LH; 31(Suppl):S261-S265 (1996)].
Whether carbohydrates elevate blood glucose and insulin depends greatly on the fiber content and the glycemic index of the carbohydrate. The distinction between simple and complex carbohydrates is less significant. White bread and potatoes are complex carbohydrates, but they have a higher glycemic index than fructose, which is a simple sugar. In one study, a high-carbohydrate, low glycemic diet resulted in 80% greater fat loss than a low-fat diet, and also reduced LDL cholesterol. A high-protein diet had the same effect on fat, but did not affect LDL cholesterol. The effect was greater for women than for men [ARCHIVES OF INTERNAL MEDICINE; McMillan-Price,J; 166(14):1466-1475 (2006)].
Low glycemic index diets can promote weight loss and maintain insulin sensitivity, whereas high glycemic index diets have the opposite effect [THE AMERICAN JOURNAL OF CLINICAL NUTRITION; Brand-Miller,JC; 76(Suppl):281S-285S (2002)]. But this effect may only apply to individuals who have a high insulin response to glucose [DIABETES CARE; Pittas,AG; 28(12):2939-2941 (2005)]. Animal experiments indicate that a high glycemic index diet is sufficient to induce high plasma insulin levels [LANCET; Pawlak,DB; 364:778-785 (2004)]. Low glycemic index diets, especially those highest in fiber, lead to less calorie over-consumption and greater insulin sensitivity [THE JOURNAL OF CLINICAL ENDOCRINOLOGY & METABOLISM; Lara-Castro,C; 89(9):4197-4205 (2004)].
Glycemic Load (GL), which is related to the amount of high glycemic index food eaten, is becoming increasingly emphasized because a tiny amount of high glycemic index food would not be expected to have a large effect [DIABETES CARE; Hodge,AM; 27(11):2701-2706 (2004)]. (For food tables of glycemic index and glycemic load see mendosa.com)
Despite the concern over HFCS, some nutrition authorities hasten to assure the public that high fructose fruits like apples are perfectly safe. Nonetheless, an observant shopper will notice how many "fruit juices" have substantial amounts of apple juice. Apple juice can be consumed 11 times faster than an intact apple and 4 times faster than apple sauce. Apple juice is deficient in beneficial fiber and is less satiating of appetite than an intact apple [JOURNAL OF NUTRITION; Stubbs,RJ; 131(10):2775S-2781S (2001)]. Whole fruits are usually to be preferred to fruit juices. (Orange juice and white grape juice contain about equal parts of fructose and glucose, but nonetheless have less fiber than whole fruit.)
Snack foods are generally high in fat and sugar because most people find these foods the most appetizing — resulting in more calorie consumption. A low-carbohydrate diet could be high in protein rather than fat. In general, protein satisfies appetite with fewer calories than do carbohydrate or fat, while reducing blood triglycerides and LDL cholesterol [INTERNATIONAL JOURNAL OF OBESITY AND RELATED METABOLIC DISORDERS; Skov,AR; 23(5):528-536 (1999) and DIABETES CARE; Parker,B; 25(3):425-430 (2002)]. The Nurses' Health Study indicated that replacing carbohydrates with protein lowers the risk of ischemic heard disease [AMERICAN JOURNAL OF CLINICAL NUTRITION; Hu,FB; 70(2):221-227 (1999)].
Concerns about bone resorption with high protein diets have not been supported in controlled studies [THE AMERICAN JOURNAL OF CLINICAL NUTRITION; Farnsworth,E; 78(1):31-39 (2003) and THE AMERICAN JOURNAL OF CLINICAL NUTRITION; Luscombe-Marsh,ND; 81(4):762-772 (2005)], but higher calcium intake could address the problem.
Although meat protein and casein (a milk protein) can cause kidney damage, whey protein (a milk protein) does not [DIE NAHRUNG; el-Sayed, MM; 42(1):12-15 (1998)]. Nor does soy protein [CURRENT OPINION IN NEPHROLOGY AND HYPERTENSION; Lentine,K; 13(3):333-336 (2004)]. (See also Does Excess Protein Cause Kidney Damage?) A meta-analysis of clinical trials indicated that about 50 grams of soy protein daily can significantly decrease serum levels of LDL cholesterol (about 13%) and triglycerides (about 10%) [NEW ENGLAND JOURNAL OF MEDICINE; Anderson,JW; 333(5):276-282 (1995)]. Whey protein is a useful adjunct to a weight loss program, to oppose loss of lean tissue rather than fat. Exercise is useful for the same purpose (see Weight Loss for CRAN).
High levels of fat in the bloodstream can impede the efficiency of insulin receptors resulting in insulin resistance, which is one of the first signs of developing type 2 diabetes. Diabetes increases the incidence of a variety of health conditions, including heart disease, neuropathy, kidney failure, etc. — increasing the likelihood of an early death. "Type 2 diabetes" (also called "non-insulin-dependent diabetes") was formerly called "adult onset diabetes". But adolescents have increasingly been developing the disease. A Cincinnati study showed a ten-fold increase in adolescent type 2 diabetes in the period between 1982 and 1994 [THE JOURNAL OF PEDIATRICS; Pinhas-Hamiel,O; 128(5 Pt 1):608-615 (1996)]. There was not a ten-fold change in genetic makeup of adolescents in that period, but there was a great increase in adolescent obesity. A study of nearly 85,000 nurses concluded that obesity is the single most important factor leading to type 2 diabetes in women [NEW ENGLAND JOURNAL OF MEDICINE; Hu,FB; 345(11):790-797 (2001)] (a result which is probably valid for men as well).
In the condition of insulin resistance insulin receptors are less responsive to insulin — the normal actions of insulin are blunted. Glucose transport into fat & muscle cells is reduced with insulin resistance resulting in elevated blood glucose. Conversion of glucose to glycogen in the liver is reduced, further elevating blood glucose. Elevated blood glucose glycates proteins, possibly including insulin receptors, thereby exacerbating insulin resistance and "accelerating aging" (diabetes is a segmental progeria). N-acetylcysteine and taurine and can prevent induction of insulin resistance by high blood glucose [AMERICIAN JOURNAL OF PHYSIOLOGY; Haber,CA; 285(4):E744-E753 (2003)]. Claims that chromium picolinate can reduce insulin resistance are the subject of considerable dispute.
In general, insulin resistance increases with age. For sedentary individuals the age-associated increase in insulin resistance is associated with an increase in body fat. Exercise can significantly improve insulin sensitivity even in very elderly people [JOURNAL OF APPLIED PHYSIOLOGY; Evans,EM; 98(1):40-45 (2005)]. Endurance-trained individuals (runners) have less insulin resistance than sedentary individuals. The increased insulin resistance of older runners compared to younger runners is not due to increased body fat, but may be due to decreased training intensity [JOURNAL OF APPLIED PHYSIOLOGY; Clevenger,CM; 93(6):2105-2111 (2002)]. Resting metabolic rate per unit of fat mass, which normally declines with age, does not decline for those who maintain their level of aerobic exercise [AMERICAN JOURNAL OF PHYSIOLOGY; van Pelt,RE; 281(3):E633-E639 (2001)].
Insulin resistance results in increased hydrolysis of triglycerides in fat cells, thereby elevating free fatty acids in the blood. High levels of free fatty acid in the blood induces insulin resistance (positive feedback). Excessive blood insulin — a consequence of insulin resistance — typically leads to dysfunction of the endothelium (the cell layer on the walls of blood vessels) [CIRCULATION; Arcaro,G; 105(5): 105(5):576-582 (2002)]. Insulin resistance leads to heart disease, in part by reducing the ability of blood vessels to regulate blood pressure (an aspect of endothelial dysfunction) [OBESITY RESEARCH; Caballero,AE; 11(11):1278-1289 (2003)]. High blood lipid means elevated LDL cholesterol and increased atherosclerosis. Insulin resistance may even reduce the capacity for high blood insulin to reduce appetite. Insulin resistance does not lead to diabetes as long as the beta−cells of the pancreas islets can continue producing increasing levels of blood insulin. Only when beta−cell production of insulin falters does diabetes appear.
The metabolic syndrome is a collection of related "metabolic disorders", the most central of which is insulin resistance. Waist circumference and elevated blood triglycerides are two additional highly correlated features. High blood pressure and low blood HDL cholesterol are also frequent features. Being "overweight" with a high BMI or high levels of fat are less central to the metabolic syndrome than is visceral (abdominal) fat. Subcutaneous fat and fat below the waist are not significant features of the metabolic syndrome. When visceral fat was surgically removed from rats at an age that was 40% of their typical lifespan they showed improved insulin action and lived about 10% longer [AGING CELL; Muzumdar,R; 7(3):439-440 (2008)]. Post-menopausal women typically develop an increased proportion of visceral fat, an effect that can be reversed by sex hormone replacement therapy [JOURNAL OF ENDOCRINOLOGY AND METABOLISM; Gambacciani,M; 82(2):414-417 (1997)].
Chronic inflammation is an important aspect of the metabolic syndrome. Healthy women with the highest levels of C−Reactive Protein (CRP, an inflammatory risk factor for cardiovascular disease) were shown to be more than 15 times more likely to develop type 2 diabetes over a 4 year period than women with low CRP blood levels [JOURNAL OF THE AMERICAN MEDICAL ASSOCIATION; Pradhan,AD; 286(3):327-334 (2001)]. Persons with the metabolic syndrome have elevated levels of inflammatory cytokines in their blood, as well as elevated levels of the coagulation-promoting protein fibrinogen. Persons with the metabolic syndrome have double the incidence of cardiovascular disease and triple the incidence of type 2 diabetes compared to the general population [JOURNAL OF ATHEROSCLEROSIS AND THROMBOSIS; Zimmet,P; 12(6):295-300 (2005)].
The prevalence of the metabolic syndrome in the United States increased in the last 3 decades of the 20th century in conjunction with a doubling of the prevalence of obesity from 15% to 30% [THE JOURNAL OF THE AMERICAN MEDICAL ASSOCIATION; Flegal,KM; 288(14):1723-1727 (2002)]. In 2002 the prevalence of the metabolic syndrome exceeded 20% for those over 20 years of age and exceeded 40% for those over 40 [THE JOURNAL OF THE AMERICAN MEDICAL ASSOCIATION; Ford,ES; 287(3):356-359 (2002)].
A 20-week experiment on rats is illustrative of the way the metabolic syndrome can develop. The control group was fed a standard rat chow whereas the experimental group was fed a diet that was 34% sucrose and 66% rat chow. Both groups were allowed to feed freely (ad libitum). The sucrose-loaded rats consumed nearly 20% more calories than the control rats. Sucrose-loading increased plasma monounsaturated fats and decreased plasma polyunsaturated fats. After 4 weeks visceral fat was about 15% higher in the sucrose-loaded rats, but after 20 weeks was more than doubled in the sucrose-loaded rats compared to the control rats. After 4 weeks plasma glucose and insulin were comparable for the two groups, but plasma triglycerides were nearly twice as high in the sucrose-loaded rats. After 20 weeks plasma glucose was still comparable for the two groups and plasma triglycerides were still doubled in the sucrose-loaded rats, but plasma insulin in the sucrose-loaded rats was about triple the level of that in the control group [EXPERIMENTAL BIOLOGY AND MEDICINE; Fukuchi,S; 229(6):486-493 (2004)].
Exercise can significantly reduce complications associated with the metabolic syndrome. Three sessions per week of 35 minutes of resistance exercise for 16 weeks by people with type 2 diabetes reduced glycated hemoglobin by 13% and reduced blood pressure from 145.2/72.6 to 135.5/69.2. 73% of the subjects were able to reduce their diabetes medications [DIABETES CARE; Castaneda,C; 25(12):2335-2341 (2002)].
Advanced Glycation End-products (AGEs) are toxic molecules formed by heating proteins, sugars and fats together. AGEs are a significant contributor to atherosclerotic disease and other diseases associated with high plasma levels of free radicals and inflammatory cytokines [JOURNALS OF GERONTOLOGY; Semba,RD; 65A(9):963-975 (2010)]. The AGE CarboxyMethyl Lysine (CML) was found to be significantly elevated in the cortical neurons and cerebral blood vessels of 25 demented subjects (selected to exclude Alzheimer's Disease) who died between the ages of 64-92 [BMC NEUROLOGY; Southern,L; 7:35 (2007)].
With dry heat, the formation of glycated proteins is greatly accelerated, and can increase the level of AGEs by as much as 200 times. Cooking with fat allows for high temperatures and also can contribute to the oxidation process that turns glycated proteins into AGEs. High temperature cooking of meat & fat produce foods with the highest AGE content [ANNALS OF THE NEW YORK ACADEMY OF SCIENCES; Uribarri,J; 1043:461-466 (2005)]. The type of cooking can make a great difference, with significantly more AGE formation from frying, broiling & grilling as compared to steaming, poaching or boiling [JOURNAL OF THE AMERICAN SOCIETY OF NEPHROLOGY; Uribarri,J; 14(3):728-731 (2003)]. About one-third of absorbed dietary AGEs (from browned foods, particularly fried poultry skin) are excreted, while the rest is presumably incorporated into body tissue [PROCEEDINGS OF THE NATIONAL ACADEMY OF SCIENCES (USA); Koschinsky,T; 94(12):6474-6479 (1997)]. High fat food has the highest AGE content (butter twice as much as olive oil), followed by high protein food (American cheese more than grilled beef). Grilled beef has nearly triple the AGE content of boiled beef. Fruits, vegetables, breads and other high carbohydrate foods have very low AGE content [JOURNAL OF THE AMERICAN DIETETIC ASSOCIATION; Goldberg,T; 104(8):1287-1291 (2004)]. A MacDonald's Big Mac has about 40 times the AGE content of a veggie burger per gram. AGEs are in cheese in proportion to fat content. Cheddar cheese (4% fat) has about 25 times the AGE content per gram of a veggie burger, but cheddar cheese with 2% fat has half the AGE content as cheddar cheese with 4% fat content [JOURNAL OF THE AMERICAN DIETETIC ASSOCIATION; Uribarri,; 110(6):911-916 (2010)].
AGEs ingested from tobacco smoke & cooked foods contribute to the metabolic syndrome and type 2 diabetes [CLINICAL DIABETES; Peppa,M; 21(4):186-187 (2003)]. Tobacco smoke is a source of AGEs, which may explain why adolescents who have metabolic syndrome are six times more likely to be smokers [CIRCULATION; Weitzman,M; 112(6):862-869 (2005)]. Dry heating of tobacco is a process called curing which dehydrates the tobacco leaves while destroying cholorophyll and oxidizing carotenoids. Starch is converted to sugar, which can glycate protein and then be oxidized into AGEs. Serum AGE levels in non-diabetic smokers has been found to be about 40% higher than in the serum of non-diabetic non-smokers [PROCEEDINGS OF THE NATIONAL ACADEMY OF SCIENCES (USA); Cerami,C; 94(25):13915-13920)].
After six months of feeding mice either a low AGE diet or a high AGE diet that was high in fat (35% fat), 75% of the high AGE mice were diabetic, whereas none of the low AGE mice were diabetic. The high AGE mice had at least twice the visceral fat and AGE-modified fat [DIABETES; Sandu,O; 54(8):2314-2319 (2005)]. In a similar experiment, after 20 weeks high AGE-fed mice had 13% more body weight, despite equal food intake. The AGE-fed mice also had twice the level of AGEs in their bloodstream [DIABETES; Hofmann,SM; 51(7):2082-2089 (2002)]. Mice fed a 50%-reduced AGEs diet had a median lifespan that was 15% longer and a maximum lifespan that was 6% longer than controls [AMERICAN JOURNAL OF PATHOLOGY; Cai,W; 170(6):1893-1902 (2007)].
In a study of non-smoking diabetic humans, two weeks of high AGE diet increased serum AGEs by 64.5% and a subsequent two weeks of low AGE diet caused a 30% decrease. Subjects on a high AGE diet for six weeks had a 86.3% increase in blood mononuclear cell TNF−α (an inflammatory cytokine) and a 35% increase in C−Reactive Protein (CRP, a inflammatory protein product), in contrast to a 20% decline in both TNF−α & CRP for those on the low AGE diet [PROCEEDINGS OF THE NATIONAL ACADEMY OF SCIENCES (USA); Vlassara,H; 99(24):15596-15601 (2002)]. Healthy human subjects given a low-AGE (30-50% reduction) diet for 4 months showed a 50% reduction in plasma markers of oxidative stress, inflammation, and AGEs [THE JOURNAL OF CLINICAL ENDOCRINOLOGY & METABOLISM; Vlassara,H; 94(11):4483-4491 (2009)]. High blood glucose potentiates the pro-inflammatory effects of AGEs, and high blood insulin further potentiates the effect of both glucose and AGEs [CIRCULATION RESEARCH; Golovchenko,I;87(9):746-752 (2000)]. Glycation of LDL cholesterol is at least as important as oxidation of LDL cholesterol in the generation of atherosclerosis [CURRENT OPINION IN LIPIDOLOGY; Younis,N; 19(4):378-384 (2008)].
In sum, tobacco smoke and cooked foods (especially meat cooked in fat) containing large amounts of AGEs can increase the likelihood and severity of the metabolic syndrome. Chronic inflammation aggrevated by AGEs can also increase the predisposition to atherosclerosis, arthritis, Alzheimer's Disease, cancer and numerous other afflictions. AGEs contribute to diabetic neuropathy, diabetic retinopathy, diabetic nephropathy (kidney failure) and aging.
Most glucose uptake by cells is by means of GLUcose Transporters (GLUT) that are either insulin-dependent (GLUT3 in neurons and placenta) or insulin-dependent (GLUT3 in muscle and fat). Free fatty acids induce insulin resistance in muscle cells by interfering with PI3K (an enzyme in the intracellular insulin signaling cascade) activity [THE JOURNAL OF CLINICAL INVESTIGATION; Dresner,A; 103(2):253-259 (1999)]. Without PI3K activity GLUT4 cannot translocate to the cell surface to bring glucose into the cells [DIABETES; McGarry,JD; 51(1):7-18(2002)]. Fat feeding, particularly saturated fat, produces insulin resistance in adipocytes (fat cells) [ATHEROSCLEROSIS; Lichtenstein,AH; 150(2):227-243 (2000)]. Healthy male volunteers fed a high fructose diet for 6 days had elevated blood triglycerides and insulin resistance [DIABETES; Faeh,D; 54(7):1907-1913 (2005)].
Visceral fat apparently induces insulin resistance by the production of the cytokine Tumor Necrosis Factor-alpha (TNF−α) from the fat cells. Obese individuals express more than twice the TNF−α mRNA & protein than do lean controls — and body weight reduction by obese individuals results in improved insulin sensitivity associated with decreased mRNA TNF−α expression [THE JOURNAL OF CLINICAL INVESTIGATION; Hotamisligil,GS; 95(5):2409-2415 (1995)]. Transgenic mice which lack fatty acid binding protein do not express mRNA for TNF−α and do not develop insulin resistance when subjected to diet-induced obesity [SCIENCE; Hotamisligil,GS; 274:1377-1379 (1996)]. One study of type 2 diabetics indicated that TNF−α does not cause insulin resistance [DIABETOLOGIA; Carey,AL; 47(6):1029-1037 (2004)], a result that is difficult to reconcile with most other studies. TNF−α induces increased free radical production from mitochondria [AMERICAN JOURNAL OF RESPIRATORY CELL AND MOLECULAR BIOLOGY; Corda,S; 24(6):762-768 (2001)]. White adipose tissue attracts macrophages, which produces the inflammatory agents (like TNF−α) associated with obesity-induced insulin resistance [JOURNAL OF CLINICAL INVESTIGATION; Xu,H; 112(12):1821-1830 (2003)]. Surgical removal of visceral fat (but not subcutaneous fat) extends the mean and maximum lifespan of rats [BIOCHEMICA ET BIOPHYSICA ACTA; Huffman,DM; 1790(10):1117-1123 (2009)]. Dietary blueberries reduce inflammatory macrophages and lipolysis in adipose tissue, increasing insulin sensitivity [JOURNAL OF NUTRITION; DeFuria,J; 139:1510-1516 (2009)].
|
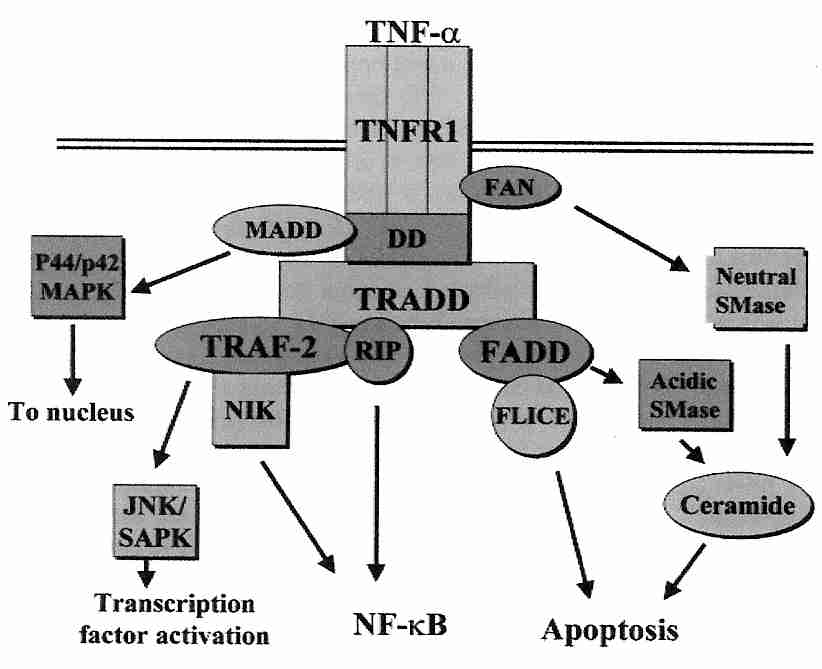
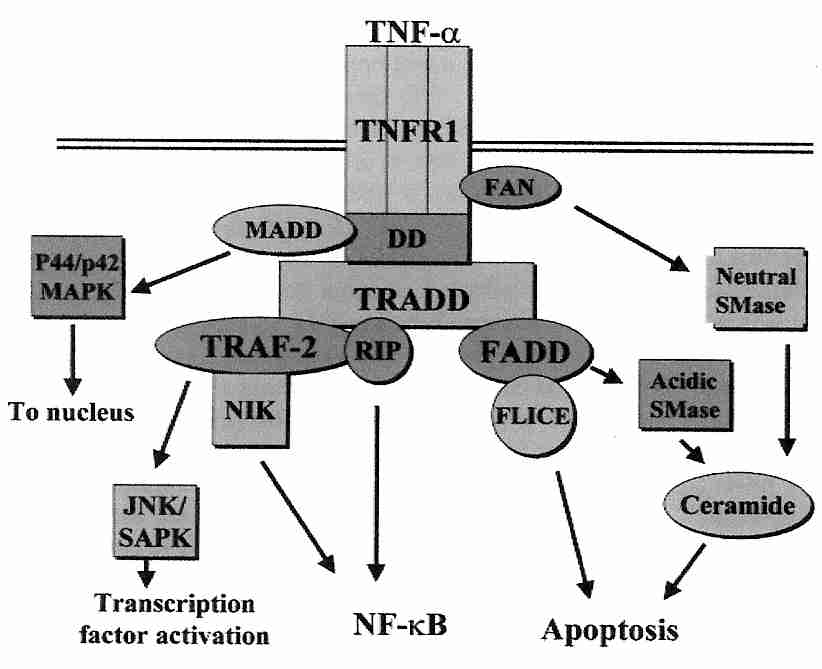
Binding of TNF−α to the TNFR1 receptor results in recruitment of TNF Receptor-Associated Death Domain (TRADD) adaptor protein, which then recruits the additional adaptor proteins Receptor-Interacting Protein (RIP), TNR−R Associated Factor−2 (TRAF−2) and Fas-Associated Death Domain (FADD), which initiates signalling. Caspase−8 recruitment to FADD can initiate apoptosis. Independent of caspase−8, FADD & RIP can induce necrosis. TRAF−2 can activate JNK (c−Jun NH2−terminal Kinase) which increases the transcriptional activity of c−Jun by phosphorylating it. RIP assists in activating NF−κB. Excessive TNF−α activity thereby contributes to inflammation and autoimmune diseases such as rheumatoid arthritis and multiple sclerosis [SCIENCE; Chen,G; 296:1634-1635 (2002)].
TNF−α activates MAPK (Mitogen Activated Protein Kinase) p38 and IKK (Inhibitor κB Kinase, which is phosphorylated by NIK, NF−κB Inducing Kinase) causing a serine phosphorylation of the insulin receptor and its associated IRS−1 (Insulin Receptor Substrate-one). These serine phosphorylations impair the tyrosine phosphorylations of those molecules which would activate PI3K and cause GLUT4 translocation [JOURNAL OF BIOLOGICAL CHEMISTRY; de Alvaro,C; 279(17):17070-17078 (2004)]. TNF−α can also catalyze the hydrolysis of membrane sphingomyelin to generate ceramide, which both inhibits GLUT4 gene transcription [BIOCHEMICAL JOURNAL; Long,SD; 319(Pt 1):179-184 (1996)] and inhibits insulin signalling on the PI3K pathway leading to GLUT4 translocation [JOURNAL OF BIOLOGICAL CHEMISTRY; Schmitz-Peiffer,C; 274(34):24202-24210 (1999)]. Another study, however, suggests that it is DAG (DiAcylGlycerol), rather than ceramide that interferes with PI3K activity [JOURNAL OF BIOLOGICAL CHEMISTRY; Yu,C; 277(52):50230-50236 (2002)]. NF−κB activation by TNF−α can protect against the apoptosis which ceramide can promote.
Down-regulation of GLUT4 expression in adipocytes is characteristic of insulin resistance. Elevation of GLUT4 expression prevents insulin resistance. PPARγ (Peroxisome Proliferator-Activated Receptor gamma) is a key transcription factor controlling the expression of GLUT4 protein [THE JOURNAL OF CLINICAL INVESTIGATION; Wu,Z; 101(1):22-32 (1998)]. Rats fed omega−3 fatty acids have significantly lower blood triglycerides & insulin than rats fed omega 6 fatty acids [THE JOURNAL OF NUTRITION; Fickova,M; 128(3):512-519 (1998)]. Eicosanoids from monounsaturated and polyunsaturated fatty acids can bind to PPARs resulting in reduced or increased insulin resistance [PROCEEDINGS OF THE NATIONAL ACADEMY OF SCIENCES (USA); Kliewer,SA; 94(9):4318-4323 (1997)]. Arachidonic acid suppresses GLUT4 expression, providing a mechanism by which omega−6 polyunsaturated fatty acids can promote insulin resistance [JOURNAL OF BIOLOGICAL CHEMISTRY; Long,SD; 271(2):1138-1144 (1996)]. Research on PPAR agonists and antagonists are promising tools for pharmacological intervention in "metabolic disease" [NATURE; Kersten,S; 405:421-424 (2000) and [THE JOURNAL OF CLINICAL INVESTIGATION; Barish,GD; 116(3):590-597 (2006)].
The trigger for the death of beta cells in the pancreas islets (and thus the trigger for type 2 diabetes) may be oxidative stress. Reactive Oxygen Species (ROS) can activate the transcription factor NF-κB resulting in the production of pro-inflammatory cytokines and inducible Nitric Oxide Synthase (iNOS) that ultimately result in beta-cell death. The anti-oxidant N−acetylcysteine can inhibit NF-κB activation and thereby attenuate type 2 diabetes [THE FASEB JOURNAL; Ho,E; 13(13):1845-1854 (1999)]. PPARγ activators are currently used to increase insulin sensitivity and decrease plasma fatty acids in patients with type 2 diabetes [THE AMERICAN JOURNAL OF MEDICINE; Kurtz,TW; 119(5 Suppl 1):24S-30S (2006)].
TNF−α also promotes the replacement of pro-inflammatory cytokines from visceral adipocytes, including InterLeukin−6 (IL−6) and InterLeukin−8 (IL−8) — inflammatory cytokines associated with obesity [EUROPEAN JOURNAL OF ENDOCRINOLOGY; Bruun,JM; 148(5):535-542 (2003)]. IL−6 is a stress-related cytokine that shows an increase in blood levels with age. IL−6 promotes the production of cortisol, fibrinogen and C−Reactive Protein (CRP) (a risk factor for myocardial infarction) [PROCEEDINGS OF THE NATIONAL ACADEMY OF SCIENCES (USA); Kiecolt-Glaser,JK; 100(15):9090-9095 (2003) and [ANNALS OF INTERNAL MEDICINE; Papanicolanou,DA; 128(2):127-137 (1998)]. Tobacco smoking can also elevate IL−6, elevate triglycerides and lower HDL cholesterol, giving smokers some of the blood profile of the metabolic syndrome [CIRCULATION JOURNAL; Yasue,H; 70(1):8-13 (2006)].
In contrast to the pro-inflammatory cytokines associated with visceral fat is the anti-inflammatory cytokine adiponectin, produced mostly by subcutaneous fat. Adiponectin reduces levels of TNF−α, CRP and vascular adhesion molecules, while increasing insulin sensitivity [TEXAS HEART INSTITUTE JOURNAL; Nesto,RW; 32(2):387-389 (2005)].